Before the patient visits the healthcare service provider, we perform a pre-insurance verification check. We get all the details of either the patient is eligible for the particular insurance, require any pre-authorization or referral, whether any copayment has to be collected, the amount of co-insurance patient shares, if the patient has met the deductible, and whether the insurance covers the service sought from the healthcare provider. This step is very important because many insurance companies do not provide retro-authorization.
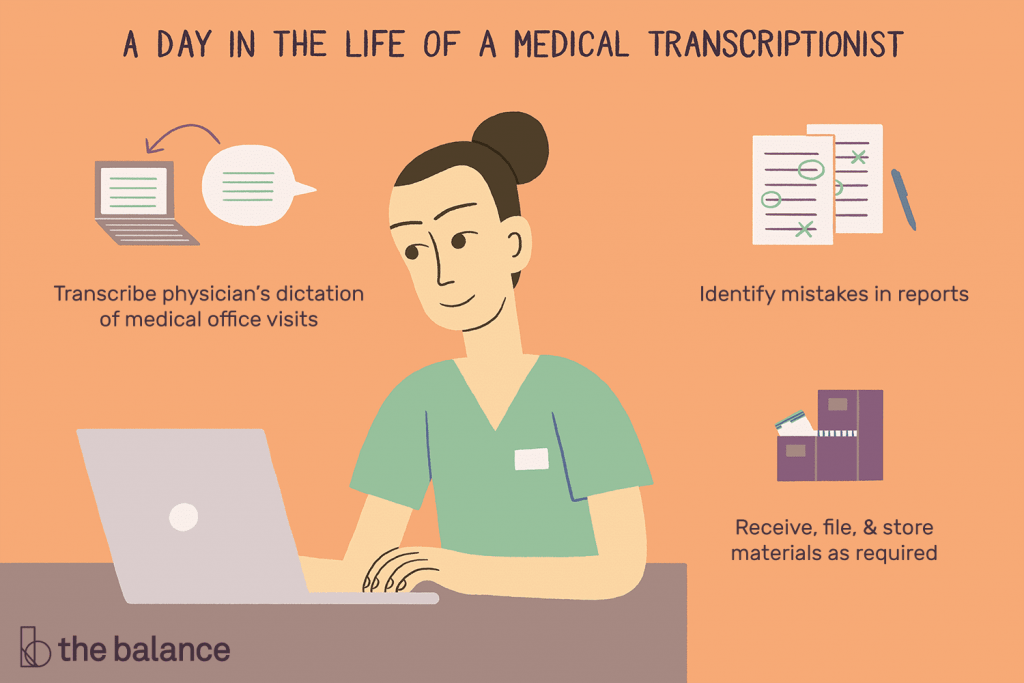
We access detailed patient’s information and bills from the healthcare service provider’s system through a secure network. All the documents are verified and validation is communicated to the respective client. After that all these medical documents are sent to the medical coding department to assign CPT and ICD codes. These coded medical documents are subjected to proof-reading and then cross-checked by the medical coding manager. After this these coded medical documents are forwarded to the charge entry team. We validate the code entered by the client as well.
Charges from coded medical documents are then entered into the particular patient account. If the patient is new and no account number exists, then a new patient account is created with all the demographic details from the patient’s registration form.
Once the details of the charges are entered and audited, the claims are then filed with the payer electronically. We process paper claims as well. Usually when the claims go through cursory filtering software to ensure that all information is contained within the document and is accurate. If any errors are caught, a paper report is sent back within 24 hours. After receiving the report, incorrect claims are rectified with the necessary and correct information within 24 hours, and after that claims are resubmitted to the insurance company.
When our experienced medical billing outsourcing professionals receive the scanned EOBs (Explanation of Benefits) and checks, these payments are then entered into the system. As part of this task, we also charge appropriate patient accounts and then immediately initiate the process for denied claims in case the actual claim is far below the expected one. Reconciliation takes place on a daily basis.
Once the claim is submitted to the payer for processing, our expert BPO follow-up team is determined to pursue all unpaid insurance claims that have crossed the 30 days bucket in order to diminish the accounts receivable (AR) days of the claim. Sometimes, the claims are underpaid and in such cases, we make sure that these claims are processed and paid correctly. The denied claims are appealed by our AR (accounts receivable) team.
The denied claims are addressed on a priority basis. Our medical billers and coders find the reason behind denied claims and refile the denial claims. Our expert on board Denial Analysts fixes the denied claim’s issue and sends them for reprocessing. If the claim requires any additional information from the provider, then these gaps are filled promptly; if the patient is responsible for denied claims, the claim is billed to the patient.
After the insurance claim is processed, we follow up with the patients for any pending balance due. A patient statement is generated and filed on a weekly, biweekly, or monthly basis, as per your healthcare business requirement. Follow-up is done through phone calls. If we do not receive any response from the patient, we move those balances to collections, generate a separate report for it, and then send it to you for further action.
Our reporting package includes monthly customized reports, insurance aging reports, and KPI (Key Performance Indicators) reports. We are offering a detailed portrayal of your healthcare practice’s financial health and the length of your claim payment cycle.
As part of our medical billing outsourcing services, after verifying that it is a case of overpayment, we can also perform credit balance processing of the patient or the payer. This ensures the correct and on-time refunds to the appropriate entity.
BJK Solutions is offering a comprehensive range of medical billing BPO services. With the chosen payer networks and government entities, we complete all applications and required paperwork on your behalf. We follow all payer contracts through to contract load date and provide copies of fully executed contracts and fee schedules to your practice or billing company. We also maintain and update the CAQH profile.